Understanding Insulin and Its Importance
Understanding Insulin and Its ImportanceInsulin is a hormone produced by the pancreas that plays a crucial role in managing diabetes. It allows your body to effectively use glucose, the primary source of energy for cells. When you eat food, especially carbohydrates, your blood sugar levels rise. In response, the pancreas releases insulin to help transport glucose from the bloodstream into the cells, where it can be used for energy.As someone with diabetes, understanding insulin and its importance is essential for maintaining healthy blood sugar levels. Without sufficient insulin or with insulin resistance, glucose builds up in the bloodstream, leading to high blood sugar levels, known as hyperglycemia. Over time, uncontrolled hyperglycemia can contribute to various health complications.In the following sections, we'll explore various aspects of insulin usage and its impact on blood sugar control. We'll delve into topics such as the timing of insulin injections, including the effects of injecting insulin after meals on post-meal blood sugar levels. We'll also discuss best practices for insulin injections, including rotating injection sites, calculating the correct insulin dose, and addressing incorrect doses. Lastly, we'll examine the benefits and considerations of mealtime insulin, exploring its role in regulating blood sugar levels and its advantages and disadvantages.By understanding insulin and its vital role in managing diabetes, you'll be better equipped to optimize your blood sugar control and lead a healthier life.
What is insulin and why is it crucial for managing diabetes?
Insulin is a hormone that plays a crucial role in managing diabetes. It is produced by the pancreas and helps regulate blood sugar levels by allowing cells in the body to take in glucose from the bloodstream and use it for energy. For individuals with diabetes, insulin therapy is necessary to compensate for the body's inability to produce enough insulin or properly utilize it.
Managing diabetes requires carefully monitoring blood sugar levels and making sure they stay within a healthy range. Insulin is crucial for achieving this goal as it helps keep blood sugar levels stable. Without adequate insulin, glucose can accumulate in the bloodstream, leading to high blood sugar levels, a condition known as hyperglycemia.
Consistently high blood sugar levels can have severe health consequences and increase the risk of complications associated with diabetes, such as cardiovascular disease, kidney damage, nerve damage, and eye problems.
By providing the body with the insulin it needs, individuals with diabetes can effectively manage their blood sugar levels and reduce the risk of complications. Insulin therapy can help control fasting blood sugar levels, as well as post-meal blood sugar levels, allowing for better overall blood sugar control.
Insulin is essential for managing diabetes because it helps regulate blood sugar levels, reduce the risk of complications, and improve overall health and well-being.
How to effectively use insulin for blood sugar control
When it comes to managing diabetes, insulin plays a crucial role in controlling blood sugar levels. Insulin is a hormone produced by the pancreas that allows your body to use glucose for energy. For individuals with diabetes, their bodies either do not produce enough insulin or cannot effectively use the insulin they produce. That's where insulin injections come in.
Using insulin effectively is essential for blood sugar control. Here are some key considerations:
- Consult with your healthcare provider: Before starting insulin therapy, it's important to consult with your healthcare provider to determine the right type of insulin for you and to establish an appropriate dosage.
- Timing is everything: Timing your insulin injections is crucial. Generally, insulin injections should be taken before meals. However, the specific timing may vary depending on the type of insulin used. Rapid-acting insulin, for example, is typically taken about 15 minutes before a meal, while short-acting insulin is taken 30 to 60 minutes before a meal. Your healthcare provider will provide guidance on the optimal timing for your individual needs.
- Follow a consistent schedule: It's important to establish a consistent schedule for insulin injections. By sticking to a routine, you can help regulate your blood sugar levels more effectively.
- Monitor your blood sugar levels: Regularly monitoring your blood sugar levels is essential for effective insulin use. This allows you to make adjustments to your insulin dosage or timing if needed.
- Balance insulin with carbohydrate intake: It's important to strike the right balance between insulin and carbohydrate intake. Monitoring your carbohydrate intake and adjusting your insulin accordingly can help ensure proper blood sugar control.
- Rotate injection sites: When injecting insulin, it's important to rotate injection sites to improve absorption. This helps prevent the development of lumps or fatty deposits beneath the skin.
- Be prepared for hypoglycemia: Taking insulin can sometimes lead to low blood sugar levels, known as hypoglycemia. It's important to be prepared for this by carrying a source of fast-acting glucose, such as glucose tablets or a sugary drink, to counteract hypoglycemia if it occurs.
Choosing the Right Timing: Before or After Meals?
Choosing the right timing for insulin injections is crucial for optimizing blood sugar control after meals. This decision can significantly impact post-meal blood sugar levels and overall diabetes management. By understanding the effects of timing on insulin action, individuals can make informed choices.
In the upcoming sections, we will explore the impact of insulin injection timing on post-meal blood sugar levels and discuss how to determine the optimal time to take insulin in relation to meals. We will also delve into best practices for insulin injections, including rotating injection sites for improved absorption, calculating the correct insulin dose, and correcting an incorrect dose.
Furthermore, we will discuss the benefits and considerations of mealtime insulin, a type of insulin specifically used to regulate blood sugar levels during meals. We will examine how mealtime insulin can help control blood sugar before, during, and after eating, as well as the advantages and disadvantages associated with its use.
By the end of this article, you will have a comprehensive understanding of the importance of choosing the right timing for insulin injections after meals in order to optimize blood sugar control and effectively manage diabetes.
How does the timing of insulin injection affect post-meal blood sugar levels?
The timing of insulin injection after a meal can significantly affect post-meal blood sugar levels in individuals with diabetes. Insulin is responsible for regulating the amount of glucose in the bloodstream, and timing its injection correctly is essential for optimizing blood sugar control.
When insulin is taken after a meal, it can help to prevent high blood sugar levels by facilitating the uptake of glucose into the cells. This is particularly important for individuals with type 1 diabetes or type 2 diabetes who require insulin injections.
By taking insulin after a meal, it aligns with the natural rise in blood sugar that occurs after eating. This helps to prevent sharp spikes in blood sugar levels and keeps them within a target range.
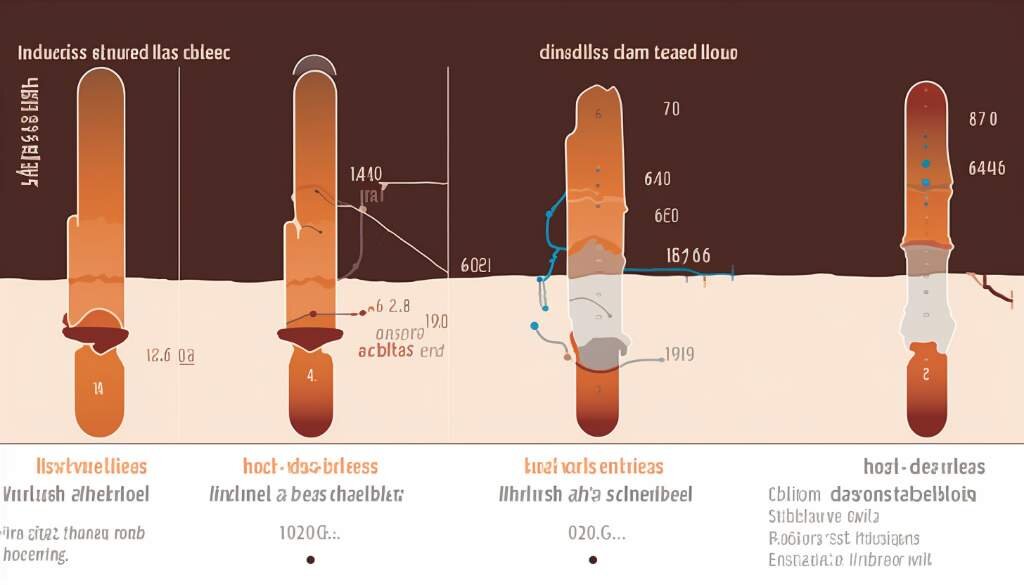
When insulin is injected after food, it starts to work within a set timeframe, usually ranging from 15 minutes to an hour, depending on the type of insulin used. Rapid-acting insulins typically start working within 15-30 minutes, while short-acting insulins may take up to an hour.
By timing insulin injections after meals, individuals can help to prevent the post-meal blood sugar surge that often occurs in people with diabetes. This can lead to improved overall blood sugar control throughout the day and reduce the risk of complications associated with high blood sugar levels.
Determining the optimal time to take insulin in relation to meals
Determining the optimal time to take insulin in relation to meals is crucial for effective blood sugar control. It can help prevent post-meal spikes in blood sugar levels and ensure that insulin is properly utilized by the body. Here are some factors to consider when deciding when to take insulin in relation to meals:
- Type of insulin: The type of insulin you are using can determine the timing of your injection. Rapid-acting insulin, such as insulin lispro or insulin aspart, should be taken around 15 minutes before a meal to match the rise in blood sugar levels caused by eating. Regular insulin, on the other hand, should be injected approximately 30 minutes before a meal to allow time for it to start working.
- Carbohydrate content of the meal: The amount of carbohydrates in your meal can affect how quickly your blood sugar rises. If you are having a meal that is high in carbohydrates, it may be beneficial to take your insulin closer to the start of the meal to ensure it starts working when your blood sugar begins to rise.
- Individual blood sugar response: Every person's body reacts differently to meals, so it is important to monitor your blood sugar levels after eating. If you notice that your blood sugar tends to spike shortly after meals, you may need to adjust the timing of your insulin injection to take it earlier to prevent the spike.
- Consultation with healthcare provider: It is important to consult with your healthcare provider or diabetes educator to determine the best timing for your insulin injections. They can provide personalized guidance based on your specific needs and lifestyle.
Best Practices for Insulin Injections
Best Practices for Insulin Injections involve several important factors that can help individuals with diabetes effectively manage their blood sugar levels. These practices are crucial to ensure proper insulin delivery, absorption, and dose accuracy. By following these best practices, individuals can optimize their insulin therapy and minimize the risk of complications.
In this section, we will explore three key areas related to best practices for insulin injections: rotating injection sites, calculating the correct insulin dose, and correcting an incorrect dose. Let's delve into each of these topics in more detail in the following sub-sections.
Rotating injection sites to improve absorption
Rotating injection sites is an important practice to improve the absorption of insulin in the body. When insulin is injected repeatedly in the same spot, it can lead to the formation of scar tissue, which can hinder the absorption of insulin and affect its effectiveness. By rotating injection sites, you can ensure that the absorption of insulin remains optimal.
Here are some key considerations when it comes to rotating injection sites:
- Choose a rotation pattern: When rotating injection sites, it's important to have a systematic plan. You can divide your injection sites into different regions, such as the abdomen, thighs, and buttocks. Create a rotation pattern that ensures you use a different site within each region for each injection, and then cycle through the regions over time.
- Avoid using the same spot too frequently: It's crucial to avoid injecting insulin in the exact same spot every time. Ideally, you should leave some space between injection sites to allow the tissue to recover and heal. This helps prevent the development of scar tissue and ensures optimal absorption.
- Monitor for any signs of skin or tissue problems: Regularly check your injection sites for any signs of skin or tissue problems. If you notice any redness, swelling, lumps, or discomfort at an injection site, consult your healthcare provider. They can determine if there is an issue and provide guidance on appropriate actions to take.
- Use proper injection techniques: Proper injection technique is essential for optimal absorption. Make sure to clean the injection site with alcohol wipes before injecting, use a new needle for each injection, and follow the instructions provided by your healthcare provider.
By rotating injection sites and following these best practices, you can improve the absorption of insulin, reduce the risk of complications, and enhance the effectiveness of your diabetes management.
Calculating the correct insulin dose
Calculating the correct insulin dose is a crucial step in effectively managing diabetes and optimizing blood sugar control. It involves determining the appropriate amount of insulin needed to maintain stable blood sugar levels throughout the day.
There are a few key factors to consider when calculating the correct insulin dose:
- Insulin sensitivity: Each individual has a different level of sensitivity to insulin. It is important to understand your body's response to insulin and adjust the dose accordingly.
- Daily carbohydrate intake: The amount of carbohydrates you consume plays a significant role in determining the insulin dose. Carbohydrates directly affect blood sugar levels, so it's important to match the insulin dose with the amount of carbohydrates consumed.
- Blood sugar levels: Monitoring your blood sugar levels regularly is essential in determining the correct insulin dose. If your blood sugar levels are consistently high or low, adjustments to the insulin dose may be necessary.
- Physical activity: Physical activity can impact blood sugar levels and insulin sensitivity. Engaging in regular exercise may require adjustments to the insulin dose to prevent hypoglycemia (low blood sugar).
It is recommended to work closely with a healthcare provider, such as an endocrinologist or diabetes educator, to determine the appropriate insulin dose. They will take into account your individual factors and help you calculate the correct insulin dose based on your specific needs and goals.
Remember that calculating the correct insulin dose is not a one-time process. It may require regular adjustments based on changes in diet, activity level, and overall health. Regular monitoring and communication with your healthcare provider are essential for maintaining optimal blood sugar control.
Correcting an incorrect insulin dose
Correcting an incorrect insulin dose is essential for maintaining optimal blood sugar control and avoiding potential complications. If an incorrect dose of insulin is taken, it can lead to either high or low blood sugar levels, depending on the situation. Here are some important considerations when correcting an incorrect insulin dose:
- Recognizing hypoglycemia: Hypoglycemia, or low blood sugar, can occur if too much insulin is taken. Symptoms of hypoglycemia include sweating, shakiness, confusion, dizziness, and weakness. If these symptoms occur, it is important to treat the low blood sugar immediately by consuming a fast-acting source of glucose, such as fruit juice or candy.
- Recognizing hyperglycemia: Hyperglycemia, or high blood sugar, can occur if too little insulin is taken. Symptoms of hyperglycemia include excessive thirst, frequent urination, fatigue, blurred vision, and slow wound healing. If these symptoms occur, it is important to adjust the insulin dose accordingly and consult a healthcare professional for further guidance.
- Consulting a healthcare professional: If an incorrect insulin dose is taken, it is crucial to consult a healthcare professional to determine the best course of action. They can provide guidance on how to correct the dose and prevent further complications.
- Monitoring blood sugar levels: Regular monitoring of blood sugar levels is essential when correcting an incorrect insulin dose. This helps to track the effectiveness of the correction and ensure that blood sugar levels are within the target range.

Benefits and Considerations of Mealtime Insulin
Mealtime insulin refers to insulin injections that are taken specifically before or after meals to help regulate blood sugar levels. It is an important strategy for individuals with diabetes to effectively manage their condition and prevent complications.
There are several benefits and considerations associated with mealtime insulin. These include:
- Improved blood sugar control: Mealtime insulin can help to regulate blood sugar levels more effectively compared to using basal insulin alone. By taking additional insulin before or after meals, individuals can better manage the rise in blood sugar that occurs after eating.
- Flexibility in meal planning: With mealtime insulin, individuals can have greater flexibility in their meal choices and timing. By adjusting the timing and dose of insulin, they can better accommodate variations in carbohydrate intake and meal schedules, making it easier to enjoy a varied diet.
- Reduced risk of hypoglycemia: By taking mealtime insulin, individuals can better match their insulin levels to their carbohydrate intake. This can help to reduce the risk of low blood sugar levels (hypoglycemia) after meals.
While mealtime insulin has several benefits, there are also some considerations to keep in mind. These include:
- Increased complexity: Mealtime insulin adds an extra layer of complexity to diabetes management. Individuals need to be mindful of timing their insulin doses correctly and monitoring their blood sugar levels closely to ensure optimal control.
- Potential for weight gain: The additional insulin doses with meals can increase the risk of weight gain. It is important for individuals to work closely with their healthcare team to find the optimal dosing regimen that balances blood sugar control with weight management.
- Need for individualization: The timing and dose of mealtime insulin should be individualized based on factors such as the individual's carbohydrate intake, activity levels, and insulin sensitivity. Regular monitoring and adjustments may be necessary to achieve optimal results.
In the following sub-sections, we will explore these topics in more detail, including how mealtime insulin can better regulate blood sugar levels and the advantages and disadvantages associated with its use.
How mealtime insulin can better regulate blood sugar levels
Mealtime insulin is an essential tool in the management of blood sugar levels for individuals with diabetes. By administering insulin before or during meals, it helps regulate glucose levels more effectively and prevent spikes in blood sugar.
One of the main benefits of mealtime insulin is its ability to mimic the body's natural insulin response to food consumption. When we eat, our pancreas releases insulin to help transport glucose from the bloodstream into our cells, where it can be used for energy. For individuals with diabetes, who either produce insufficient insulin or have cells that are resistant to its effects, mealtime insulin can help bridge this gap.
By injecting insulin before a meal, it becomes available in the bloodstream at the same time as the ingested carbohydrates, allowing it to work alongside the body's natural insulin response. This helps prevent a rapid rise in blood sugar after eating, as the mealtime insulin assists in transporting the glucose into the cells.
Mealtime insulin also offers the flexibility to adjust and match the insulin dose to the amount of carbohydrates ingested. This helps maintain stable blood sugar levels, as the insulin dosage can be personalized based on factors such as carbohydrate content, current blood sugar levels, and anticipated activity levels after the meal.
However, it's important to note that mealtime insulin should always be used under the guidance of a healthcare professional. Determining the ideal dosage and timing will depend on an individual's specific needs, which may require adjustments over time.
Advantages and disadvantages of mealtime insulin
Mealtime insulin, also known as prandial insulin, is a type of insulin that is taken specifically to help regulate blood sugar levels after meals. It can be beneficial for individuals with diabetes who struggle to maintain their blood sugar within a healthy range after eating. However, like any medical treatment, there are advantages and disadvantages to consider.
Advantages of mealtime insulin:
- Better blood sugar control: One of the main advantages of mealtime insulin is that it can help individuals achieve better blood sugar control after meals. By taking insulin specifically timed with meals, the medication can work to lower blood sugar levels more effectively.
- Flexibility in meal choices: Mealtime insulin provides greater flexibility in meal choices since it can compensate for the carbohydrates consumed. Individuals on mealtime insulin can have a wider variety of foods and still maintain optimal blood sugar levels.
- Reduces the risk of post-meal spikes: By taking mealtime insulin, individuals can significantly reduce the risk of post-meal blood sugar spikes, which can be dangerous, especially for individuals with diabetes. It helps ensure that blood sugar levels return to a safe range more quickly and effectively.
- Convenient dosing: Mealtime insulin is usually administered in a single dose directly before or after meals, making it a convenient option for individuals who have a consistent mealtime routine.
Disadvantages of mealtime insulin:
- Increased risk of hypoglycemia: One potential disadvantage of mealtime insulin is an increased risk of hypoglycemia (low blood sugar) if the dosage is not accurately calculated or timed. It requires careful monitoring and adjustments to avoid this potential side effect.
- Injection discomfort: Since mealtime insulin is typically injected using a syringe or pen, some individuals may experience injection discomfort or anxiety associated with injections.
- Timing challenges: Taking mealtime insulin requires careful timing to ensure that it is administered close enough to mealtimes for optimal effectiveness. For individuals with irregular eating habits or unpredictable meal schedules, this can prove to be challenging.
It is important for individuals considering mealtime insulin to consult with their healthcare provider to understand the potential benefits and risks based on their unique situation. The advantages of better blood sugar control and more flexibility in meal choices may outweigh the disadvantages for many individuals, but it is crucial to have a comprehensive understanding of these factors before starting mealtime insulin therapy.
Summary
Summary: In this section, we will provide a summary of the key points discussed in the article on timing insulin injections after meals. We will discuss the importance of understanding insulin and its role in managing diabetes. We will also explore the impact of timing insulin injections on post-meal blood sugar levels and how to determine the optimal timing in relation to meals. Furthermore, we will provide best practices for insulin injections, including rotating injection sites, calculating the correct insulin dose, and correcting an incorrect dose. Lastly, we will cover the benefits and considerations of mealtime insulin for better blood sugar regulation. Stay tuned for valuable insights on optimizing blood sugar control through the timing of insulin injections after meals.
Key takeaways on the importance of timing insulin injections after meals
Timing insulin injections after meals is crucial for optimal blood sugar control in individuals with diabetes. Here are the key takeaways on the importance of timing insulin injections after meals:
- Taking insulin after meals helps match the timing of its effect with the rise in blood sugar levels that occurs after eating. In individuals with diabetes, the body either does not produce enough insulin or is unable to effectively use the insulin it produces. By injecting insulin after meals, the exogenous insulin can help regulate blood sugar levels by facilitating the uptake of glucose into the cells.
- Taking insulin after meals can help prevent post-meal blood sugar spikes. When individuals with diabetes consume carbohydrates, their blood sugar levels tend to rise. This is known as postprandial hyperglycemia. Injecting insulin after meals helps prevent these spikes by regulating the uptake of glucose, preventing blood sugar levels from climbing too high.
- Timing insulin injections after meals allows for greater flexibility in meal patterns and enhances dietary freedom. By injecting insulin after meals, individuals with diabetes can have more freedom in the timing and quantity of their meals. This is particularly advantageous for individuals who follow flexible meal plans or have irregular eating patterns, as they can adjust their insulin dose based on the amount of carbohydrates consumed during the meal.
- Injecting insulin after meals helps reduce the risk of hypoglycemia. Hypoglycemia, or low blood sugar, is a potential risk when administering insulin. By taking insulin after meals, the risk of hypoglycemia is minimized since the insulin's peak action aligns with the post-meal rise in blood sugar levels.